A Brief History of Gas Chromatography
 Gas chromatography (GC) is one of the most important and prevalent analytical tools available to chemists. It was invented in 1952 by A.T. James and A.J.P. Martin as an outgrowth of research dating back to the previous decade.1-6 Their early techniques on adsorption and partition enabled some of the later developments that A.J.P. Martin spoke about at the 1957 Lansing Symposium, entitled, “Past, Present and Future of Gas Chromatography.” He concluded his address with the following prediction: “If we tie the gas chromatograph to other pieces of laboratory equipment, we have the possibility of almost the automatic chemist…”2 While the idea of an “automatic chemist” hasn’t quite come to fruition, Martin’s belief “that the uniting instrument of the gas chromatograph in the center” of his lab of the future certainly has.2 With the meteoric rise of GC7, its adoption and adaptation continued unabated in the ensuing decades. Then, “The introduction of robust, efficient, and reproducible fused-silica capillary columns and the provision of relatively inexpensive but reliable equipment for GC-MS provided a crucial new impetus in the 1980s.”1 Interestingly, the GC column saw some major advancements within just a few miles of AMPAC Analytical Laboratories. At that location, Walter Jennings and the company he co-founded, J&W Scientific, were instrumental in the development and manufacturing of capillary GC columns. The company was eventually purchased by Agilent in 2001.8,9
Gas chromatography (GC) is one of the most important and prevalent analytical tools available to chemists. It was invented in 1952 by A.T. James and A.J.P. Martin as an outgrowth of research dating back to the previous decade.1-6 Their early techniques on adsorption and partition enabled some of the later developments that A.J.P. Martin spoke about at the 1957 Lansing Symposium, entitled, “Past, Present and Future of Gas Chromatography.” He concluded his address with the following prediction: “If we tie the gas chromatograph to other pieces of laboratory equipment, we have the possibility of almost the automatic chemist…”2 While the idea of an “automatic chemist” hasn’t quite come to fruition, Martin’s belief “that the uniting instrument of the gas chromatograph in the center” of his lab of the future certainly has.2 With the meteoric rise of GC7, its adoption and adaptation continued unabated in the ensuing decades. Then, “The introduction of robust, efficient, and reproducible fused-silica capillary columns and the provision of relatively inexpensive but reliable equipment for GC-MS provided a crucial new impetus in the 1980s.”1 Interestingly, the GC column saw some major advancements within just a few miles of AMPAC Analytical Laboratories. At that location, Walter Jennings and the company he co-founded, J&W Scientific, were instrumental in the development and manufacturing of capillary GC columns. The company was eventually purchased by Agilent in 2001.8,9
GC Capabilities
Some of the analyses that GC can do include the separation of compounds in mixtures based on the polarity of the compounds, testing for purity – or for impurities, e.g., and detection of residual solvents. Conversely, with a technique known as preparative chromatography, GC can be used to prepare pure compounds from a mixture. In pharmaceutical analysis, there are additional applications:
- Analysis of various functional groups.
- Determining purity of pharmaceutical compounds.
- Analysis of drugs that are commonly abused.
- Determination in pharmaceutical R & D the identity of natural products that contain complex mixtures of similar compounds.
- Use in metabolomics studies.10
GC for Testing Residual Solvents
The testing of residual solvents is necessary to ensure potency and, with some solvents, to determine their potential negative effects. GC is an excellent choice to do this. Residual solvents are separated into three classifications by the ICH (International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use):
Class 1 solvents: Solvents to be avoided – Known human carcinogens, strongly suspected human carcinogens and environmental hazards. The Permissible Daily Exposure (PDE) of these solvents used in pharmaceutical products can range from 2 to 1500 parts per million (PPM).
Class 2 solvents: Solvents to be limited – Non-genotoxic animal carcinogens or possible causative agents of other irreversible toxicity such as neurotoxicity or teratogenicity and solvents suspected of other significant but reversible toxicities. The PDE for these solvents ranges from 50 to 3880 ppm.
Class 3 solvents: Solvents with low toxic potential – low toxic potential to man requiring no health-based exposure limit. Class 3 solvents have PDEs of 50 mg or more per day.11
Within these three classifications, some of the most commonly used solvents are listed:
- Benzene (class 1)
- Acetonitrile, Cyclohexane, Hexane, and Methanol (class 2)
- Acetic Acid, Acetone, and Heptane (class 3).11,12
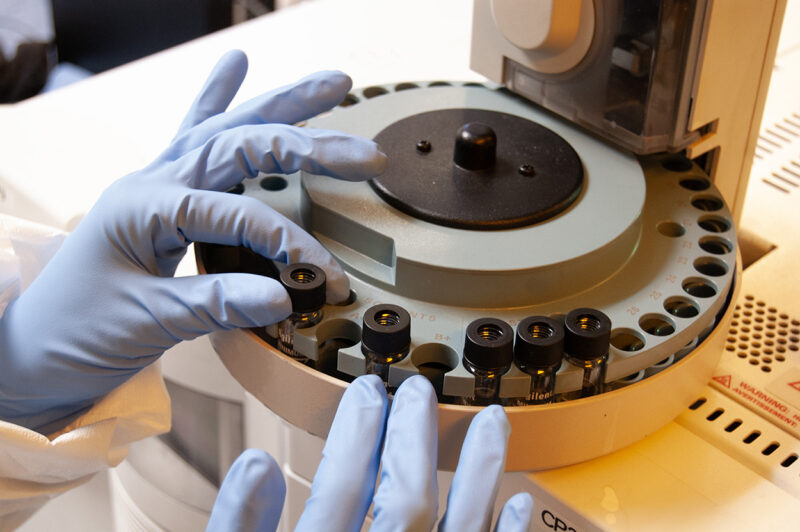
Headspace GC (HSGC) and Direct Injection GC
In addition to the numerous GC developments such as column type, phase and coating techniques, and multidimensional GC, two types of sampling methods arose: direct injection (“DI”) and headspace (“HSGC”). In the former, the sample is injected “directly” into a typical sample injector of the GC column. In HSGC, when heated, “the more volatile compounds will tend to move into the gas phase (or headspace) sample. The more volatile the compound, the more concentrated it will be in the headspace. Conversely, the less volatile (and more GC-unfriendly) components that represent the bulk of the sample will tend to remain in the liquid phase.“13
Therefore, by extracting the “headspace vapor and injecting it into a gas chromatograph, there will be far less of the less-volatile material entering the GC column, making the chromatography much cleaner, easier, and faster.”13 Generally, HSGS is much cleaner and results in less wear on the column. For more on comparative techniques with DI and HSGC, please see the first entry in the “Resources” section below.
We Can Assist with your GC Needs
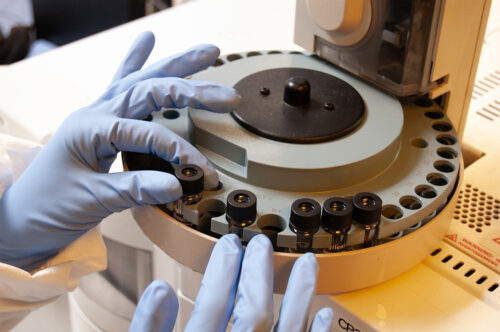
AMPAC Analytical has years of experience and numerous experts in Gas Chromatography who can assist with method development for analyses for both common and atypical sample matrices that will allow you to stay ahead of evolving regulatory concerns. Please contact us with any specific questions or to receive a quote for your GC needs.
References
- History of Gas Chromatography – ScienceDirect
- The Development of Gas Chromatography – ScienceDirect
- Gas-Liquid Chromatography: the Separation and Identification of the Methyl Esters of Saturated and Unsaturated Acids from Formic Acid to n-Octadecanoic Acid (PDF)
- James A T & Martin A J P. Gas-liquid partition chromatography: the separation and microestimation of volatile fatty acids from formic acid to dodecanoic acid. Biochem. J. 50:679-90, 1952. (upenn.edu)
- A New Form of Chromatogram Employing Two Liquid Phases – PMC (nih.gov)
- Gas Chromatography | SpringerLink
- Three Early Symposia Showing the Direction for the Evolution of Gas Chromatography.pdf
- Co-Founder of J&W Scientific, Gas Chromatography Pioneer Walter Jennings Dies | Agilent
- Professor Walter Goodrich Jennings: A Remembrance (chromatographyonline.com)
- Pharmaceutical Applications of Gas Chromatography
- https://database.ich.org/sites/default/files/ICH_Q3C-R8_Guideline_Step4_2021_0422_1.pdf
- ICH_Q3C-R8_Guideline_Step4_2021_0422_1.pdf
- An Introduction to Headspace Sampling in Gas Chromatography Fundamentals and Theory (perkinelmer.com)
Resources
- Considerations for The Analysis of Organic Volatile Impurities in Pharmaceutical Products
- Highly sensitive gas chromatographic analysis of ethanol in whole blood, serum, urine, and fecal supernatants by the direct injection method | Clinical Chemistry | Oxford Academic (oup.com)
- Quantitative analysis of methanol in wastewater by GC-MS with direct injection or headspace SPME sample introduction – Analytical Methods (RSC Publishing)
- Comprehensive Two-Dimensional Gas Chromatography as a Bioanalytical Platform for Drug Discovery and Analysis

 The path to successful drug discovery and development is extremely long, expensive, and risky and can take between 10 to 15 years at an average cost of more than $1–2 billion for every new drug that is approved for clinical use.
The path to successful drug discovery and development is extremely long, expensive, and risky and can take between 10 to 15 years at an average cost of more than $1–2 billion for every new drug that is approved for clinical use.


 Forced Degradation is an important addendum to our
Forced Degradation is an important addendum to our 




 Elemental impurities in food have been in the news recently, with reports of everything from lead being found in baby food to arsenic, cadmium, and assorted heavy metals in dark chocolate and other foods.
Elemental impurities in food have been in the news recently, with reports of everything from lead being found in baby food to arsenic, cadmium, and assorted heavy metals in dark chocolate and other foods.

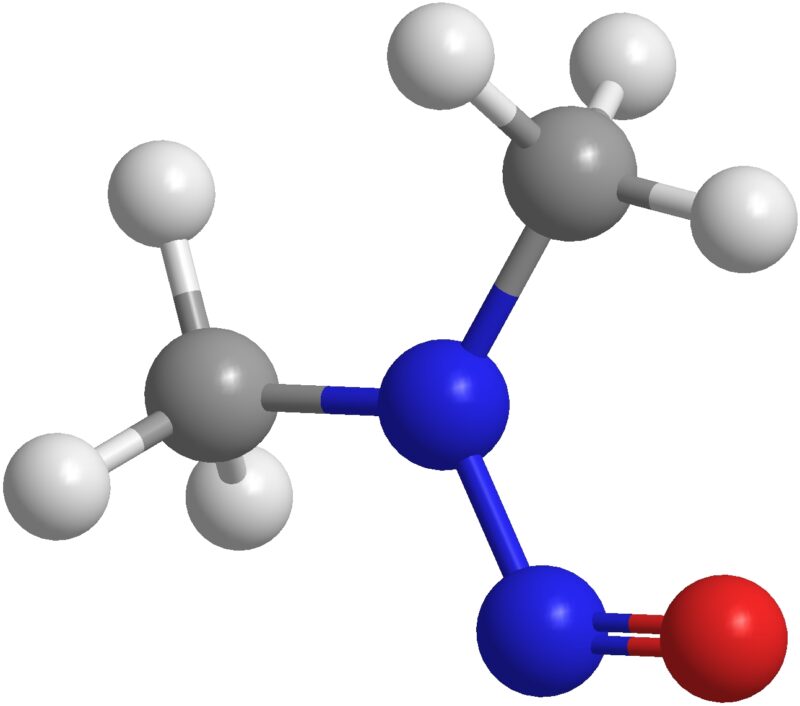
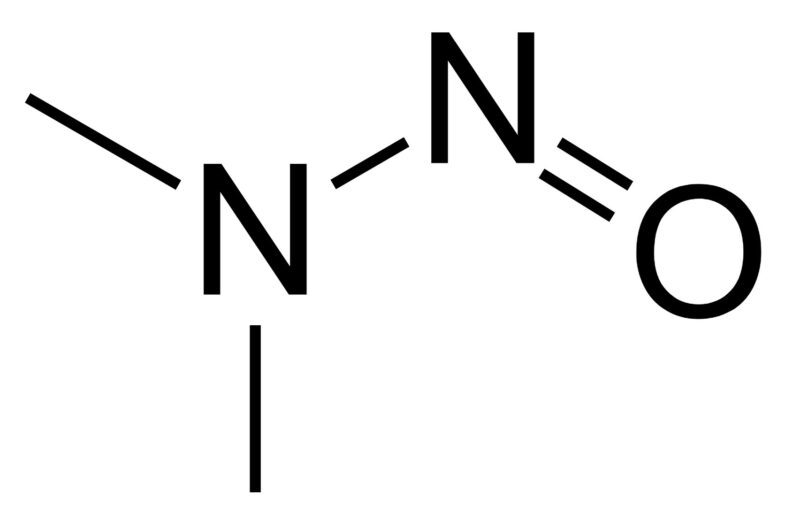
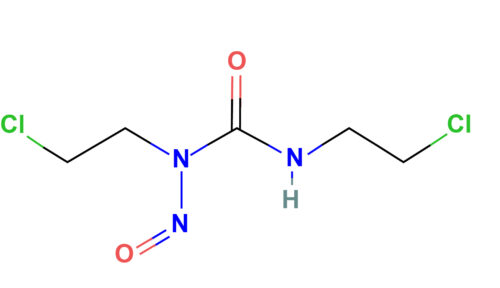
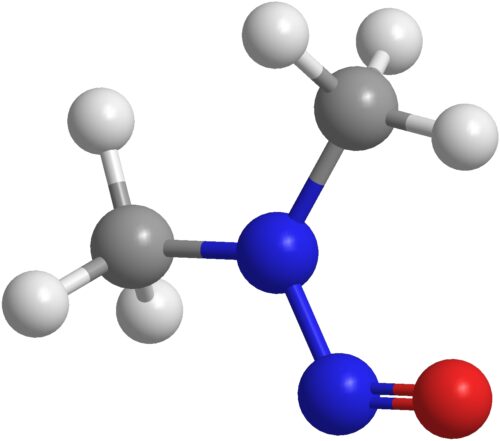 NDMA
NDMA